Living with sickle cell disease (SCD) can feel like a constant battle that affects millions of people worldwide—especially those of African, Middle Eastern, and South Asian descent. The unpredictable chronic pain, the relentless fatigue, frequent hospitalisations, and the worry about long-term organ damage can cast a long shadow over daily life. For decades, researches focused on easing symptoms, but what if there was a way to change the very course of the disease? What if there was a potential cure? Bone marrow transplant for sickle cell disease (BMT), also known as a sickle cell stem cell transplant.
This revolutionary procedure offers a profound hope for individuals living with SCD, aiming to replace diseased cells with healthy ones and potentially freeing them from the chronic struggles of this genetic condition. In this blog, we’ll explore what a bone marrow transplant for sickle cell entails, who might be a candidate, the process, and what life looks like after this life-changing treatment.
What is Sickle Cell Disease? A Brief Overview
Before we dive into BMT, let’s briefly understand SCD. Sickle cell disease is an inherited blood disorder caused by a genetic mutation in hemoglobin, the protein in red blood cells that carries oxygen.. Normally, red blood cells are round and flexible, moving easily through blood vessels to carry oxygen to the body’s tissues. However, in SCD, a genetic mutation causes red blood cells to become stiff and sticky, and shaped like a crescent moon or “sickle.”
These misshapen cells struggle to pass through tiny blood vessels, leading to blockages that cause impaired blood flow (vaso-occlusion), oxygen deprivation (ischemia),shortened red blood cell lifespan (anemia), recurrent pain, and progressive organ damage and strokes, and a host of other debilitating complications. While treatments like hydroxyurea and regular blood transfusions help manage symptoms, they don’t address the root cause – until now.
Bone Marrow Transplant: The Path to a Cure
A bone marrow transplant for sickle cell, also known as a hematopoietic stem cell transplant is currently the only known cure for sickle cell disease.
5 easy Steps to Get Treated Abroad

Share Case Details

Get Expert Opinion and Hospital Quotes

Get Visa Invitation & Hotel Recommendations

Get Received At Airport and Start Your Treatment

Travel Back and Get Followups Through Us
The core idea behind the sickle cell stem cell transplant is simple yet profound: replace the diseased bone marrow – where blood cells are made – with healthy, functioning stem cells from a donor. These new, healthy stem cells will then “engraft” in the patient’s bones, beginning to produce normal red blood cells free from the sickle cell mutation.
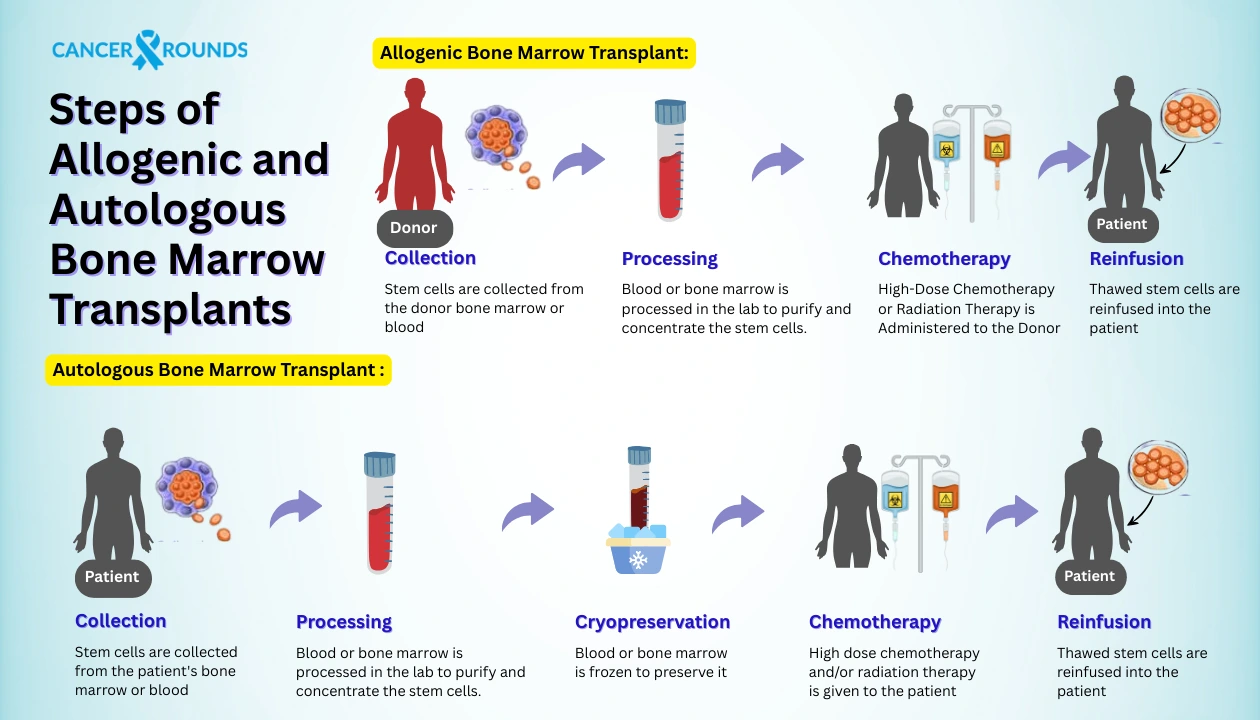
Based on the source of the donor cells, there are main types of bone marrow (or stem cell) transplants used for treating sickle cell anemia.
First comes, the allogeneic transplant, meaning the stem cells come from another person. This could be a perfectly matched sibling, a partially matched relative (haploidentical transplant), or even an unrelated donor found through registries
The matched sibling donor transplant, also known as allogeneic transplant from a matched sibling, is currently the gold standard for curing sickle cell anemia, especially in children. This type of transplant involves using bone marrow or stem cells from a fully HLA-matched brother or sister, which occurs in about 25% of full siblings. It offers the highest success rate—with cure rates reaching 85–90%, particularly in young patients who have not yet suffered severe organ damage and a lower risk of complications, such as graft-versus-host disease (GVHD), because of the close genetic match. However, not everyone has a matched sibling, which limits its availability. Even when a match is found, the patient must undergo intensive pre-transplant conditioning and take immunosuppressive drugs post-transplant to ensure success.
When a sibling match isn’t available, doctors may turn to a matched unrelated donor—someone found through an international donor registry. This is known as: Allogeneic transplant from a matched unrelated donor. This transplant type involves more risk than MSDs due to less genetic similarity, and as a result, success rates are generally lower, with a higher likelihood of rejection or GVHD.
Finding a perfect donor match is particularly challenging for patients from ethnic minority backgrounds, who are underrepresented in donor registries. While this option can be life-saving for some, it is often reserved for patients with severe complications and no family donors, due to the increased risk of side effects. Doctors typically only recommend MUD transplants in cases where the potential benefits outweigh the risks.
A haploidentical donor transplant uses stem cells from a family member—such as a parent, child, or sibling—who is only a 50% genetic match. This option has become more viable in recent years thanks to advances in transplant techniques that help prevent rejection and manage complications like GVHD. Although still considered experimental, early studies show promising results, and it is increasingly available through clinical trials.. As research continues, this option may become more mainstream.
Another one is a Bonus option, autologous transplant using Gene Therapy. An exciting new frontier in treating sickle cell disease involves gene therapy, which offers a potential cure without needing a donor. In this method, doctors collect the patient’s own stem cells and genetically modify them in a lab to correct or bypass the sickle cell mutation. After preparing the patient with chemotherapy, the edited cells are infused back, and the body begins to produce healthy red blood cells.
Because the cells come from the patient themselves, there’s no risk of donor rejection or GVHD, and no need for a donor match. However, gene therapy is still in the clinical trial phase, and long-term safety and durability are still being studied. While not widely available yet, it represents a huge breakthrough in the search for a universal cure.
Suitable Candidate for BMT?
Deciding on a bone marrow transplant for sickle cell is a complex, deeply personal choice, and not everyone with SCD is a candidate. The decision is made in close consultation with a dedicated team of hematologists and transplant specialists.
Key factors considered include:
- Age: Generally, younger patients (children and adolescents) tend to have better outcomes, though adult transplants are becoming more common with refined protocols.
- Disease Severity: Patients with frequent pain crises, acute chest syndrome, stroke, or significant organ damage may be prioritized.
- Donor Availability: The presence of a suitable matched sibling or unrelated donor is critical.
- Overall Health: The patient must be healthy enough to withstand the intensive bone marrow transplant procedure for sickle cell and its potential side effects.
The medical team performs a thorough evaluation to determine if a stem cell transplant for sickle cell is the right, and safest, option for you or your loved one.
BMT Process: Step-by-Step
The bone marrow transplant procedure for sickle cell is a multi-stage journey that requires immense courage and patience.
This is often the first and most critical step is donor search and matching after diagnosis. Doctors search for a donor whose Human Leukocyte Antigens (HLA) closely match the patient’s. A perfect or near-perfect match from a sibling usually offers the best chance of success, but national and international registries have expanded the pool of unrelated donors.
The patient undergoes pre-transplant evaluation which includes a rigorous series of tests – blood work, imaging, organ function assessments, and psychological evaluations – to ensure they are healthy enough for the procedure.
Then comes, conditioning regimen, perhaps the toughest part. Patients receive high-dose chemotherapy (and sometimes radiation) over several days. The goal is to eliminate their existing, sickle-producing bone marrow and suppress their immune system to prevent rejection of the new cells.
This is the “new birthday!” The Transplant Day (Infusion), the healthy donor stem cells are infused into the patient through an IV line, much like a blood transfusion. It’s a remarkably quick and painless part of the process.
After the infusion, the focus is post-transplant recovery & monitoring. This is basically a waiting period, typically weeks, in a specialized hospital unit. During this time, the patient’s immune system is severely compromised, making them highly vulnerable to infections. The medical team closely monitors for “engraftment,” which is when the new stem cells settle into the bone marrow and start producing healthy blood cells. Patients will also receive immunosuppressive drugs to prevent Graft-versus-Host Disease (GVHD), a potential complication where the donor cells attack the recipient’s body.
Risks and Benefits of BMT for SCD
Like any powerful medical intervention, a sickle cell bone marrow transplant comes with both significant benefits and potential risks.
Potential Benefits:
- A true cure
- Improved quality of life
- Increased lifespan and improved long-term health outcomes.
- No more transfusions/Hydroxyurea
Potential Risks:
- Graft-versus-Host Disease (GVHD)
- Infections
- Organ Toxicity
- Relapse
- Infertility
It’s crucial to have open and honest conversations with your transplant team about these risks and how they are managed.
Life After BMT: What to Expect
The journey doesn’t end when you leave the hospital. Life after a sickle cell stem cell transplant involves continued care and adjustments. Patients will undergo long-term follow-up with their transplant team, gradually reducing immunosuppressive medications over time. Regular check-ups are essential to monitor for any late complications and ensure sustained health.
While the path to full recovery can be long – sometimes a year or more – many patients eventually experience a remarkable return to a more normal, active life, free from the shadow of sickle cell disease. It’s a transformative experience, offering a second chance at life for many individuals and their families. Support groups and psychological counseling can be invaluable during this period of adjustment.
Conclusion
The advancements in bone marrow transplant for sickle cell disease represent a ray of hope for thousands affected by this challenging condition. While it is an intensive and complex bone marrow transplant procedure for sickle cell, the possibility of a cure is a powerful motivator. If you or a loved one are living with SCD, discuss the potential of a sickle cell bone marrow transplant with Cancer Rounds. It’s a journey of courage, but one that offers the incredible promise of a healthier, brighter future, free from the burdens of sickle cell disease.
 Chat on WhatsApp
Chat on WhatsApp